Masks are a controversial topic right now. Many people want to know the truth on masks and if they really are effective in preventing the spread of COVID-19. As is typical with COVID related information we see and hear in the media and read on social media, much of that information is incorrect. If you are into following the science, listen to someone who actually has the credentials to speak intelligently on the subject, Dr. Stephen Petty. He is a forensics, exposures and PPE expert.
Below is video of Dr. Petty presenting on PPE and Aerosols. The original video was censored and removed by YouTube. Considering that he is highly credentialed and is a true “expert” in this field, that shouldn’t be the case. Dr. Petty holds both a B.S. and an M.S. in Chemical Engineering, both with honors. He has an M.B.A. He was a Senior Research Scientist at Battelle and the Senior Research Engineer at Colombia Gas. He has a CIH national certification, as well as a C.S.P. certification and is a licensed Professional Engineer in many states, including Ohio, Florida, Pennsylvania, West Virginia, Kentucky and Texas. He has served as a national exposure/PPE expert in hundreds of cases, including Monsanto Roundup and DuPont C-8. He’s also an Adjunct Professor at Franklin University and holds 9 U.S. Patents. He holds membership in all the Industrial Hygiene professional associations, as well as the American Institute of Chemical Engineers. This is why he is regarded as the most renowned expert in this field and why he is the true expert when it comes to wearing masks. Here’s a different YouTube video which contains most of the original censored presentation.
Video Transcript
[Dr. Stephen Petty]: Just a quick introduction. My name is Stephen Petty, and my educational background is undergraduate and graduate degrees in chemical engineering out of Washington in Seattle, and then MBA here in Dayton. Spent ten years at Patel as a senior research are scientists and 10 years at Columbia Gas and then 25 in my own company.
[Dr. Stephen Petty]: I guess for the last 20 years, I’ve been an exposure PPE warnings expert, and most recently, I’ve been retained as an exposure expert for all these Monsanto Roundup cases. So I’m one of the top testifying experts on exposure and PP in the US.
[Dr. Stephen Petty]: In a previous lifetime, I had nine US patents and HPC systems, so that was a different life. But with that, if we could go on to Slide six.
[Dr. Stephen Petty]: I want to talk just briefly about the field of industrial hygiene because it’s largely not understood by the public. I guess they’ve never heard about it. Most people have heard of medical doctors. They’ve heard of dentists. They haven’t heard of industrial hygienist or industrial hygiene, which sounds like maybe we work in dentist offices or something, but it’s a completely different field, and it’s the science and devoted to the anticipation, recognition, evaluation and control of things that make people feel better, sick or killer. And so it’s a very interesting field.
[Dr. Stephen Petty]: We’re basically exposure experts. We try to figure out why anticipate control, why people are getting sick and what might be hurting them.
[Dr. Stephen Petty]: For instance, I got called to the Blue Jackets players. When one gets sick, a lot of them get sick. So I went down and investigated their locker rooms to figure out why that was happening. So it’s a field… what’s most irritating to me is you get a lot of medical doctors to pontificate on exposure PPE and they really don’t have training in that dimension.
[Dr. Stephen Petty]: I always say, well, would you have your dentist to your heart surgery may well be that they’re very smart people and they know a lot. But heart surgery isn’t their discipline. Well, most medical, in fact, in litigation, we always have at least two disciplines. The exposure PPE expert. That’s me. And then we have the causation expert, which is a medical doctor. And so there are two different disciplines.
[Dr. Stephen Petty]: And unfortunately, we have a lot of people pontificating on PPE, personal protective equipment and exposure, and they really don’t have the right background to do.
[Dr. Stephen Petty]: So we could keep on going. Let’s go to slide 9. I’m going to skip around. And by the way, I spoke to give him some credit, I spoke on Daniel Horowitz’s podcast for an hour on March 5, so that for your listeners, you may want to listen to that because I talk about the psychology of what’s going on now as well.
[Dr. Stephen Petty]: Exposure is really quite simple. And many things I’ll talk about today are simple, but simple things aren’t well understood I gathered. The key on exposure is these things: Time to a toxin, less is better. Concentration, lower is better, and distance further is better.
I’m here to tell you the six foot rule. I don’t know what science that comes from, but as I’ll show you, it makes no sense.
[Dr. Stephen Petty]: Next slide, if you will. Just to summarize what I’m going to tell you today and probably in the next 15 minutes, personal protective equipment is the least desirable way to protect people, mainly because it’s uncomfortable and people don’t wear it properly.
[Dr. Stephen Petty]: You see this with evidence and masks are not personal protective equipment. So what you see is these people, when they wear masks are down below their nose. They’re all with facial hair. It’s a joke. The other thing that’s going on is that the science is really suggesting that the material of concern are these small aerosols. And remember, we started with surfaces, surfaces, surfaces. Then we went to droplets, droplets, droplets. And now you’re starting to see some science crack out there and say, maybe aerosols, aerosols, aerosols. Well, I’m here to tell you, I did calculations a year ago in March saying aerosols, aerosols, aerosols. So instead of being surfaces, droplets, aerosols, it should have been aerosol, aerosol, aerosol.
[Dr. Stephen Petty]: And the reason is that these smaller particles and I can tell you that from experience in working with silica and asbestos and other where I’ve actually testified, even if there’s a spectrum of sizes of particles, the little ones are most concerned because they get into the deep one, whereas the larger droplets either fall to the ground or they get taken up by the mucus tissues and don’t get as deep. And the other thing I’m going to talk about is the way that you deal with this issue is use the concept called engineering controls. And in this case, the key is dilution and destruction. We’ll talk about that later.
[Dr. Stephen Petty]: Next, please. This is a great little chart. It’s called the Hierarchy of controls to minimize exposures. This is a fundamental concept in industrial hygiene that’s been around for 100 years, and what it does is list the things you want to do first and last in order to control people’s exposures.
[Dr. Stephen Petty]: The first one, substitution or elimination, really doesn’t apply to code, but that would be if you have a really hazardous material to substitute with a less hazardous material. That doesn’t apply here. The next most effective thing you can do is what we call engineering controls, and that is for any particular contaminant or hazard. Either dilute it, destroy it or contain it. Well, it’s kind of hard to contain COVID, really. So the keys here are dilution destruction.
[Dr. Stephen Petty]: The next one is administrative controls, which means this limit the time in spaces. I’m here to tell you that the place you’re going to get diseases in indoor spaces, not outdoor spaces. When I heard people like the governor of New York say, Well, we want to keep everybody indoors, don’t go to the park, don’t go to the beaches. I want to pull my hair out because the place I want them is outside, not inside, because everybody knows that contaminants build up indoors, not outdoors.
[Dr. Stephen Petty]: And the last and least effective in this hierarchy of controls is PPE respiration or protecting the lungs. That would be respirators and mass don’t even fall on this list of controls. That’s the interesting point.
[Dr. Stephen Petty]: Okay, next. And these are real respirators here’s. The half. The one on the right is a half faced one and the bottom of the barrel is an N-95. They’re, I guess, technically a respirator, but not a very good one. Masks don’t even fall in that category.
An interesting story. I came down from Ohio to Florida yesterday, and I was wearing my half face respirator and two thirds of the way down, for the third time, I was told that I had to remove it and put on a little thin surgical mask. And I tried to explain to the people that I was an expert in PPE and that I was protecting myself. They were insistent that they would not let me fly again unless I put on this little mask. And I pointed out to the flight attendant, I said, you see those gaps where I could stick my finger through your mask. You have no protection.
[Dr. Stephen Petty]: But….it was useless. So I had to take it off and put on. Fortunately, I had an N-95 as a backup, but this is how insane it is out there.
[Dr. Stephen Petty]: Let’s continue. Osha either is misleading at best or dishonest at worst. Here’s a slide that shows on page one. They say they recommend they always say recommend. They don’t say require. “We recommend you wear a mask, but you go into page six, and it says some interesting things. Surgical masks are not respirators, and they might provide the same level of protection to workers as properly fitted respirators”. In fact, they provide almost no protection, and “cloth face coverings are also not acceptable substitutes for respirators“. This is a passive admission, as it should be, as I say to people, if I ever recommended in court that people say being exposed to asbestos fibers should be protected by wearing a mask, I probably would lose all my credentials. And same with Silica. And so OSHA knows this. I always say it’s not that they’re not smart. They’re just dishonest. In my opinion. If you read to page six, then all of a sudden you get the truth. But it’s a little, I think at best it’s disingenuous to say we recommend wearing a mask and then tell people six days later in the fine print, well, they really aren’t very protective.
[Comment from participant Dr. Frank]: When you say silica, you’re talking about, like, coal dust and things like that, right?
[Dr. Stephen Petty]: No. Silica is actually sand. What happens in coal mines is the coal seam is trapped between layers of sand or silica. And what’s happened in another story. But because coal was for a while being increasingly mined in thinner seams, they were cutting more silica. And as a result, we had the rates of silica exposure quadruple in the 90s. But it’s basically sand particles grounded very small.
[Comment from participant Dr. Frank] Right. I knew what it was because I’m a chemist, too. I know what SiO₂, is, but I wanted the definition of silica for our listeners.
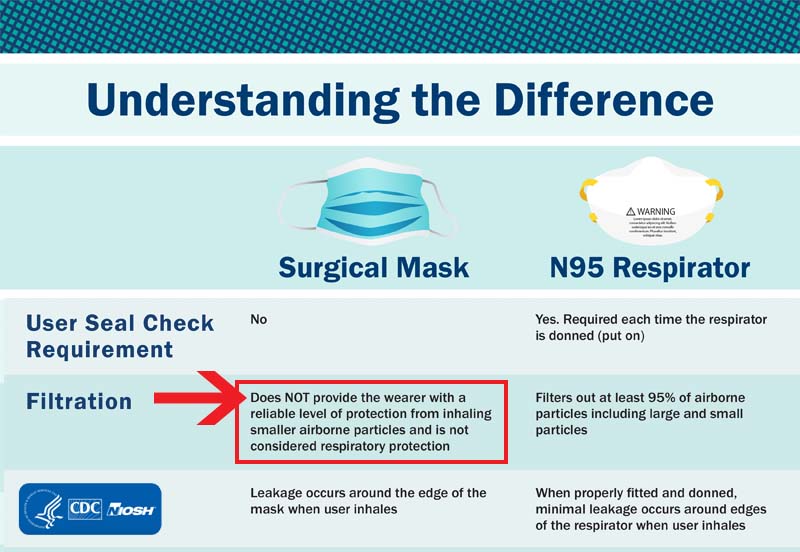
[Dr. Stephen Petty]: Then if we go to the next one, CDC is really no better. I found this on their website. I blew it up on the right. And I said: Masks versus Respirators.
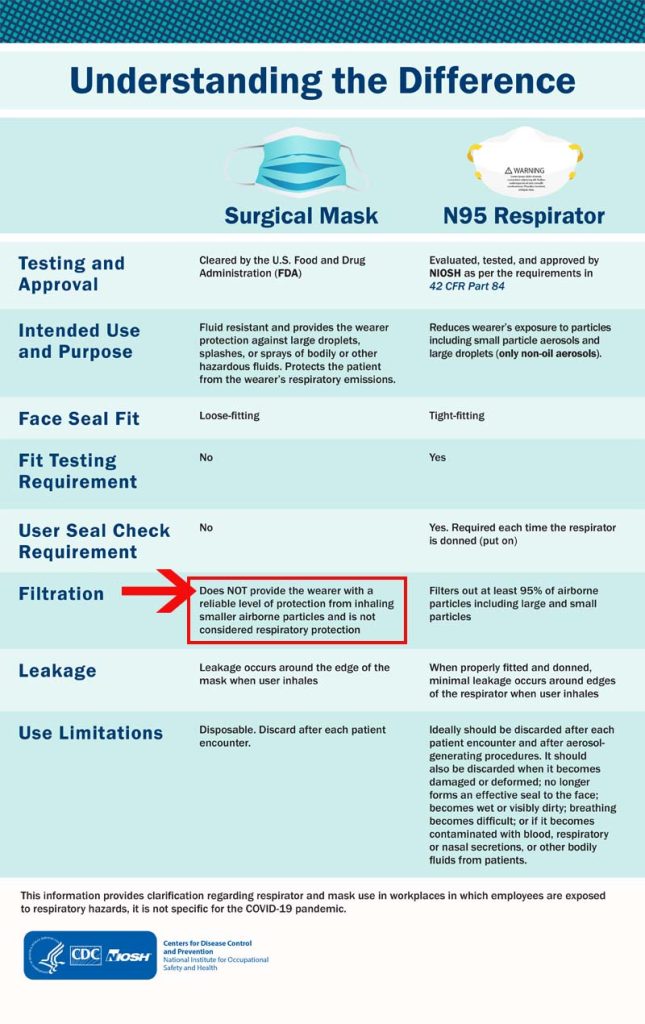
I won’t read at all. But it says on masks “does not provide the wearer with a reliable level of protection from inhaling smaller airborne particles and is not considered respiratory protection.“
Well, if it’s not, why are we wearing it?
“Leakage occurs around the edges of the mask when user inhales.“
[Dr. Stephen Petty]: I’ll get to this in a bit, but there’s no seal with the mask. That’s the problem. It’s a freeway for anything to come and go. And when they say, well you protect others, even if it doesn’t protect you or vice versa… I said does the little virus care whether it goes through the window opening on one side or the other?
[Dr. Stephen Petty]: So I thought, Well, it’d be fine. Osha has a respiratory protection standard, right? It’s called OSHA 29 CRF 1910.134.
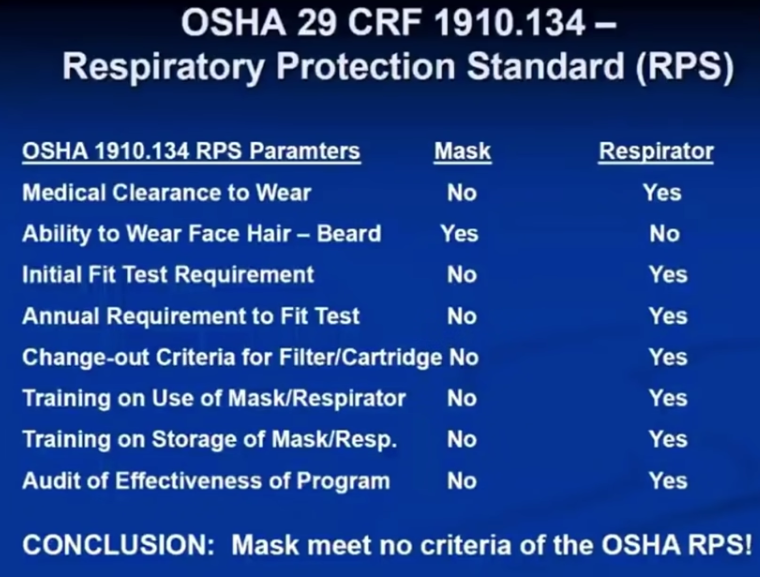
[Dr. Stephen Petty]: I testify on it dozens of times, if not hundreds. I said, Well, let’s compare the primary requirements under the OSHA respiratory protection standard, which would be the standard we would consider for protecting our lungs.
[Dr. Stephen Petty]: Well, under the respiratory protection standard, do you need a medical clearance in order to wear a respirator? Absolutely. You got to make sure that you’re healthy enough to wear one. Masks? No.
[Dr. Stephen Petty]: Can you wear facial hair like a beard or a mustache? Respiratory protection set? No. Mask. Sure, see them all the time.
[Dr. Stephen Petty]: You need a fit test? No, not for a mask. So you go down this list. There isn’t a single criteria that I find of the main criteria of the respiratory protection standard, where mask fits their criteria.
[Dr. Stephen Petty]: Go ahead. So what OSHA say about droplets versus aerosols? And I’ll get to the definition of these in a second. But it says this is where they’re really dishonest. And I’ll show you why. In a second, they say that it’s most likely your exposure is likely due to droplets, although some people might have exposure to aerosols for which PPE is required. Well, this is the little dance that’s going on. And I’m here to tell you that if they ever admit that the primary mechanism of exposure is aerosols, the mask and the six foot rule are dead. So this is why they’re very nervous about the term aerosol. Go ahead.
[Comment from participant Kathryn Huwig] The one thing I’d like to put in there as well when they talked about it being aerosolized as well, it cracked me up because, well, if it’s aerosolized, then we were all exposed last year. If it’s droplets. Okay, if it’s aerosolized, that’s great news. We were exposed. Everybody was exposed all the time.
[Dr. Stephen Petty]: They were, they were. There’s a National Academy of Sciences Press article that came out last month, and this is busy, but I want to walk you through it. This is a graph for monkeys breathing in the size of particles. So on the far right hand side, you’ll see that what they do is they provide on the bottom is pre-infecting the monkey. And then these are days after they infected the monkey, one, three, seven and 14. And up this side is a log plot. That’s what’s a little dangerous of the number of particles that they count. So this high bar is 10,000 particles, then 1000 in the middle, then 110, and then one. And you see up here, it’s a little hard to see. But these individual bars all have to do with the size of the particles from 0.3 microns to 5 and then 10. So you can see that the tens are like one to eight particles, whereas the 0.3 microns are like 10,000. So the definitions are that aerosols are less than five microns. Droplets are five to ten microns. So what does this chart really say? It says that when they did monkey studies measuring the size of particles released pre-getting sick, and then after giving them COVID, what is the distribution of particles they’re breathing out in terms of size and quantity. And it’s clear that the little guys, I call them the aerosols, the little guys, as people can understand, the little guys. And they’re by far dominant, at least in this work, which is very recent. And there’s other work that says the same thing. They’re by far the dominant number of particles, and they’re by far the small ones.
[Dr. Stephen Petty]: So let’s go to the next one. Yeah, we can ignore that. Go ahead. That’s booboo on my part.
[Dr. Stephen Petty]: So I thought, Well, everybody wants to know what the heck’s a micron.
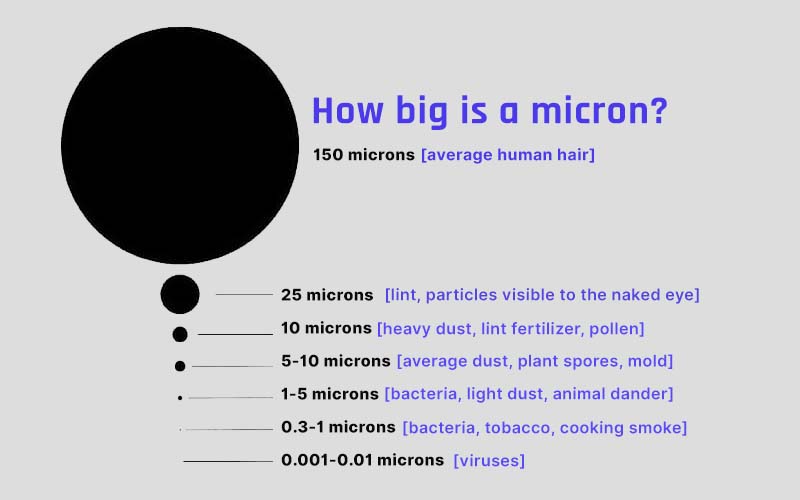
[Dr. Stephen Petty]: So I said, okay, and this, I don’t know if you can have a cursor on it. But if you look at the black ring, the big circle, imagine that that’s the cross section of a human hair. And then if you look at this little dot, this little red dot, I can’t get one kind of at 04:00 inside the circle. That red dot is the cross sectional area of a micron.
So a micron has 4,000 times less area than a human hair. And mind you, that the virus is as low as 1/10 of a micron in terms of size. So I ask people, do you think you can slide a human hair by the side of your mask. Everybody says yes. And I said, do you think that little guy can get by there then? And I said, do you think the little guy cares whether he’s incoming or outgoing? So this is very, I would say, if you want to begin to prove to people how stupid masks are, go this graph of this cross section of human hair versus a micron. And a micron is a big guy.
[Comment from participant Dr. Frank]: That’s right. Because in your previous graph, you showed that the aerosol particles that mattered were 0.3 microns.
[Dr. Stephen Petty]: Well, the next slide is going to really hammer at home. Anyway, no, keep going. We’ll skip over that bottom.
[Dr. Stephen Petty]: The study basically said they concluded, that study I cited with all the graphs that, hey, we got to worry about the little guys. So this is a little bit busy, but there’s a thing called Stokes law, and it’s a calculation where you can decide what’s the velocity of a particle if you release it, given its diameter and given its density, how fast does it fall? So what I thought would be interesting is let’s take different diameter particles, and specifically, let’s assume it’s got the density of covid, and how long would it take to fall 5 feet, which would be kind of the distance from somebody’s mouth to the floor. And I did this a year ago in March. And what you find is, yeah, for droplets that are ten or 25 on the bottom left, 10, 25, 100 microns, they’ll fall to the ground in something like 1 minute to nine minutes. But look what happens when you get to particles that are 0.5 microns to a 1/10th of a micron. The time to fall is somewhere between 1 day and 59 days. And in fact, the virus itself is around 0.1-0.3. So we’re looking at these little guys that stay suspended and still air from seven to 50 days. So here’s the problem. The little guys are always a problem because one they can get to the deep lung. But the other problem is they stay in the air for a long, long time. So in fact, you can have a scenario if the ventilation is bad indoors, but they actually accumulate. And so you could be an aisle four of a store and somebody had been sick two days earlier. And that stuff still floating around. Remember, these calculations assume still air. You know what happens if you see dust particles, which are like 25 microns. If you see in the sunlight, right, you’ll see them dancing around sometimes by your window. And when you go through them, you’ll see them kind of all move around. Well, anytime you have movement of air, it’s going to re-suspend this material. So the problem with these aerosols is they stay in the air for a long time. So, how in the world does 6ft have any meaning any meaning? It has no meaning.
[Dr. Stephen Petty]: So again, why are these aerosols so important? Well, first of all, they’re very small. The term aerosols is often mixed in medical terminology with respirable particles respirable always being five microns or less. Well, why do they call them respirable? Because they get to the deep lung. And the other problem is that they can stay suspended for hours to days. The bottom line is this really renders this 6-foot rule and these masks useless. I mean, I get asked the question all the time, the lawyer question, are you saying they have zero effectiveness? And I’ll say, Well, here’s my parable for that answer. I said, you got a mathematician and an engineer in a room and they’re looking at the far wall. And they’re asked by the moderator the following question, series of questions. Walk to halfway towards the wall. Everyone walks halfway. Walk there half again. So now we’re a quarter of the distance. And I say, and walk to this wall half the distance, forever. Do you get to the wall? And the mathematician says theoretically, no. And the engineer says yes, close enough. So when I asked the question to mask help at all, I said, It may not be zero, but it’s damn close.
[Dr. Stephen Petty]: The analogy I give, and it’s probably an overly fair analogy because I don’t think it’s even this close. Imagine you built a wall out of chain link fence, and that represents a mask. And imagine that around the wall you have window or door openings, but there’s no windows or doors present, I said. And imagine the virus is a nat, which I’m probably being generous. Does anybody really believe the nat can’t get through the chain link fence? But more importantly, can it get through the open window openings that have no restriction at all? And then somebody asked me…well another good analogy to this is let’s imagine we have a tank of water because we got two resistances here. The chain link fence and the open windows. Say we got a big container of water and we have a six-inch opening and a one-inch opening. Well, which opening do you think most of the water goes through when you open the valves? All right. Next.
[Dr. Stephen Petty]: This Academy of press thing says while the majority of particles exhale look like they’re aerosols, and it looks like they’ll get right through the mask. And they certainly are going to go further than 2 meters. And also that the little guys seem to be the marker for disease. No surprise cause they get the deep lung. Go ahead.
[Dr. Stephen Petty]: I think we’ve gone backwards. So this is not going to be easy to read. But on February 15, a bunch of physicians wrote to the White House and Fauci etc. about this whole aerosol issue. And I’m going to spend some time here because it’s important. They recognize this is the sleeping giant, which is aerosols.
[Dr. Stephen Petty]: So within there, they say it has been clear that transmission through inhalation of small aerosol particles is important in a significant mode of transportation…transmission I should say. Numerous studies have demonstrated that aerosols can remain in the air and viable for long periods of time and travel long distances within a room, and sometimes further. I’ve already shown that that’s true. This is a major group of scientists telling Fauci and the White House “we got a problem here, folks”.
[Dr. Stephen Petty]: Gathering indoor spaces without adequate ventilation puts them at high risk. Not a surprise indoors, poor ventilation, maximum concentration, it says. But on the bottom, most CDC guidance and recommendations have not yet been updated or strengthened to address and limit inhalation exposures to small aerosol particles. I think this is being generous to these folks. I don’t believe for a second that what I’m telling you and has been known for decades, they don’t have knowledge of.
When you look at the science of masks, it’s clear that they don’t make sense. So you have to say, well, what’s the reason for it? I think it goes to the behavioral side, which is, politicians and public officials wanted to do something and the something was tell people to wear a mask and tell people that will help. And so people naturally want to do something to help each other. And so they buy into this argument. My only thought on this whole thing was, why the hell didn’t they say, let’s put in the engineering controls of inhalation and destructive devices. That will make a big difference. But instead they did this mask thing and I find it almost unconscionable.
[Dr. Stephen Petty]: The CDC says, this is the scientists, not me, “CDC continues to use outdated and confusing term. Respiratory droplets describe both larger propelled droplets and the smaller inhalable aerosol particles“. And they also say that the transmission is they don’t consider the inhalation exposure via the same aerosols at short distances. In other words, these aerosols, what they’re really saying is when you hear the word aerosols, I always say the small guys. And the small guys are the problem, and I think everybody has known it. But this is beginning to crawl out from the scientific community because there are some honest brokers out there.
[Dr. Stephen Petty]: This artificial distinction needs to be replaced, but up to date terminology, including inhalation of small aerosols. This is my statements here in the bold. CDC guides and recommendations do not include control measures. No, I didn’t say this. This is their last conclusion. I’m sorry. I apologize. The next to last paragraph. CDC guidance and recommendations do not include the control measures necessary for protecting the public and workers from inhalation exposure to SARS-CoV-2. Then I write at the bottom, Aerosol: the kingpin word that renders mask and the 6-foot roll essentially meaningless.
[Dr. Stephen Petty]: Now it doesn’t help to just be a critic, because nobody likes someone who is just a critic and says everyone is wrong, but remember back to this hierarchy of controls. There are things we can do. We can use engineering controls first, not masks. The keys are, and I’ve been telling people this for years, on the dilution side, on the ventilation for buildings, increase the fresh air ventilation. Set the fresh air dampeners to maximum opening. I had a situation where it was one of the few coin club shows in Ohio. Ohio state coin show in September. We held it and I got a lot of resistance. But I went to the hotel and I said, I want, they had a big ballroom, I said I want those vents in the ceilings with fans wide open and I want you to override the energy controls in your hvc system, so we had maximum ventilation. And it was like a wind tunnel in that building. And I’ll tell you what, we didn’t have a single reported incident. Now maybe that’s anecdotal but the engineer for the hotel said to me “That’s brilliant”. And I said, “No, it’s common sense.” And I said, why don’t we chew up a little bit of energy. Because the energy codes have tightened up our buildings so much so that there is very little fresh air. I said let’s have a directive where we’re going to override these energy code requirements, and we’re going to chew up some electricity or gas. And we may have some humidity control issues, but we’re going to maximum ventilate commercial and industrial facilities. And that would have made a heck of a difference. Especially if these things are aerosols where they float around. On the ventilation side, crack a window or a door whether it be at your home or work or whatever. Yea you’re going to chew up some electricity. But in these times why not. And then secondly I said, meet outside. People if you’re in your homes, meet outside when you can or crack or open your doors. That’s real advice that will make a difference.
[Stephen Petty] The destruction side of it. There is a technology that I do believe works. Although I tell all my friends, wouldn’t have been nice if we had spent even a fraction of these trillions of dollars looking at destruction technology instead of giving everyone $1,400 bucks or whatever they’re getting. Why don’t we, for $400 bucks plus $200 to install them, why don’t we tell the HVC companies, we’ll give you $600 bucks if you install these devices in everybody’s home that want one. They supposedly destroy 99.9% of viruses, bacteria and mold. And near as I can tell they don’t side effects like ozone or other technologies.

[Stephen Petty]: And everyone says, as you’re sure you’re right? And I say I’d like to have a fraction of the money they’ve wasted on masks and other things to prove it. But I say, I think based on what I’ve been able to learn in my experience, they work. Remember the PPE is the least desirable option. The masks aren’t PPEs. I always talk about this. If we want an emotional argument, instead of saying “masks, masks, masks”, let’s go “dilution destruction, dilution destruction!”.
[Stephen Petty]: So just to close, the same story. Masks are not PPE. It’s the little guys that count, because they stay in the air a long time and they can get into the deep lung. And by God, let’s start using under the industrial hygiene hierarchy of controls, let’s include engineering controls which include dilution and destruction.
One reply on “Do Masks Work to Prevent the Spread of COVID-19? [Mask Expert Dr. Stephen Petty]”
We collectively let our top scientists give us unscientific recommendations. So when our leaders say trust the science, Hitler also said this. I get fit tested for my respirator annually since 1982 as do many pest control techs which I’ve been. Its nice to see that some Dr’s are not afraid of truth